Shoulders
Treatments targeted at specific conditions.
Most shoulder injures involve the muscles, tendons and ligaments rather than the bones. As many of the conditions mimic one another, shoulder injuries are notoriously difficult to diagnose and can be painful for long periods of time. Seeing an osteopath early in the injury timeline means that we can diagnose and treat the injury quickly, avoiding chronicity and resulting in a better prognosis.
Athletes and manual labourers are particularly vulnerable to shoulder injuries, but we also see many patients who have suffered shoulder injuries during every day activities such as gardening, painting or being pulled by the dog!
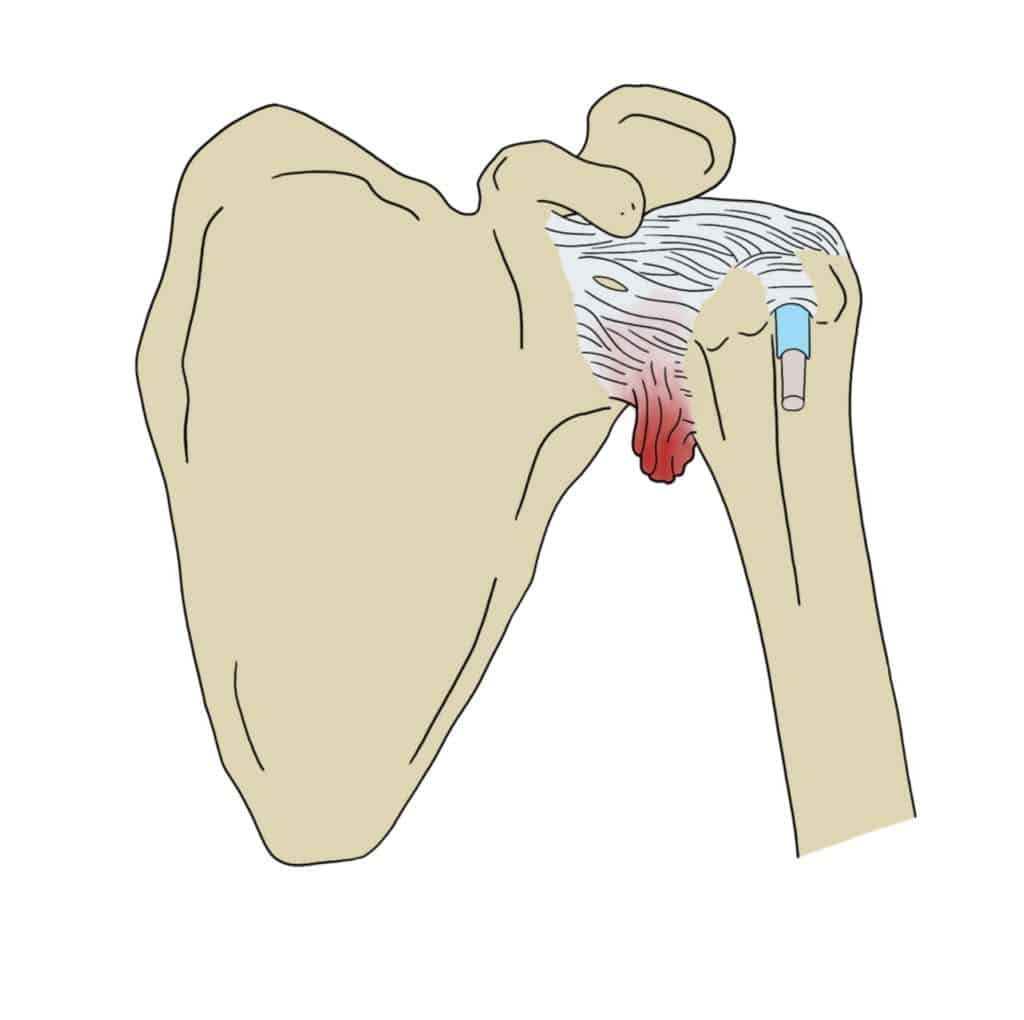
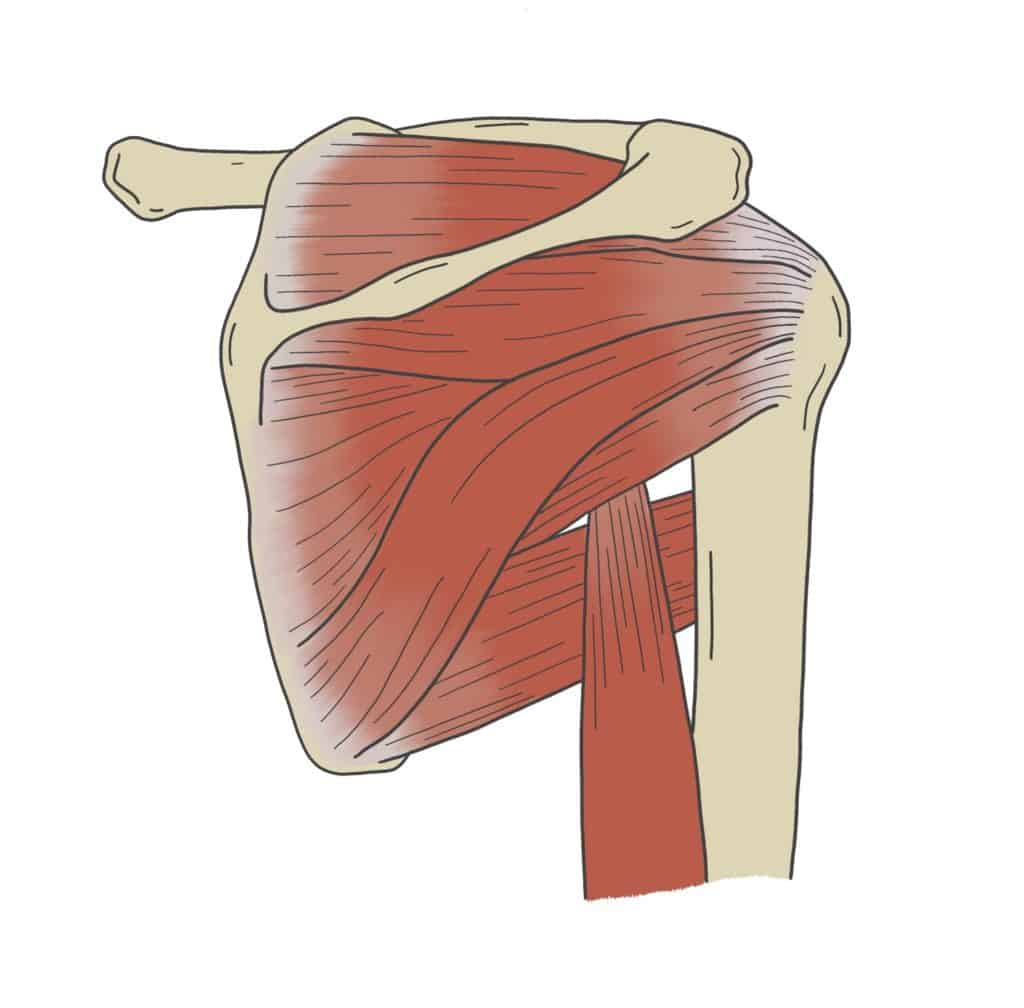
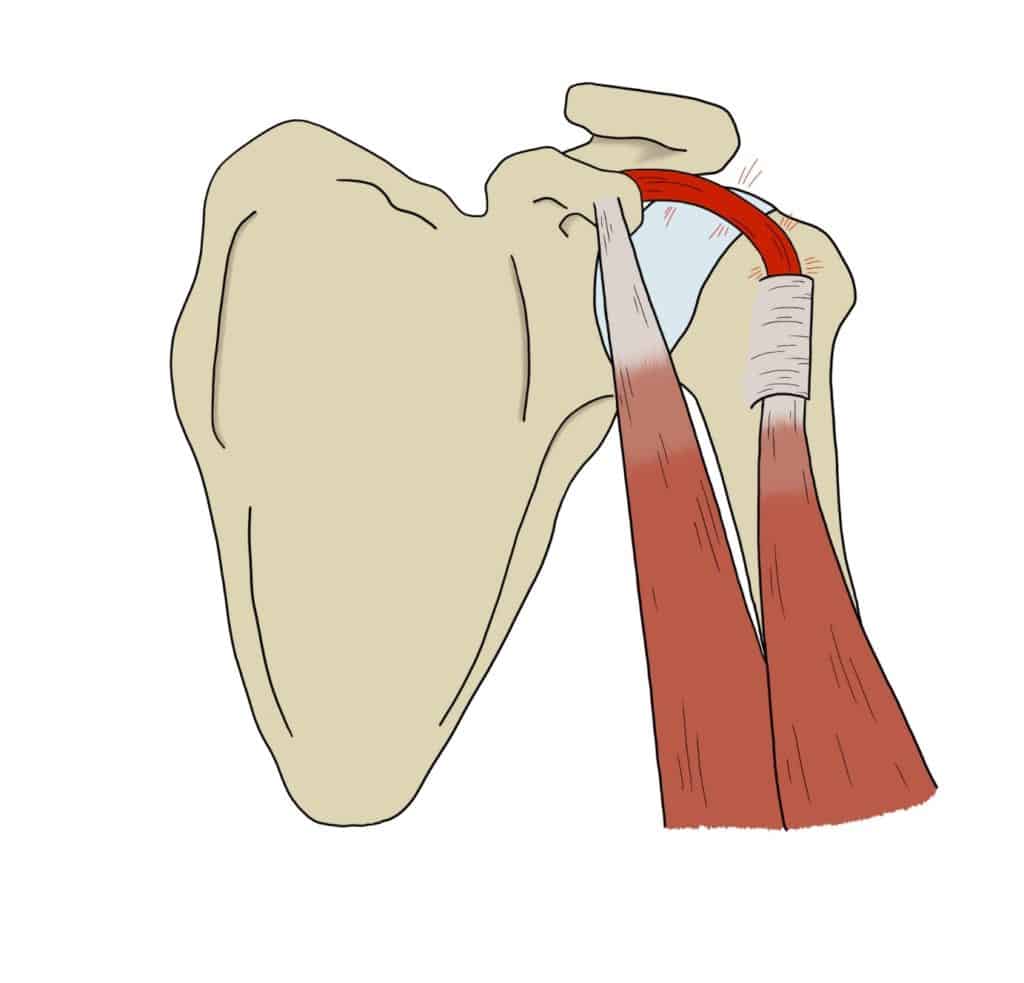
Rotator Cuff Injuries
Rotator cuff injuries are one of the most common problems that patients present with at the clinic. The rotator cuff muscles are a group of four small muscles that surround your shoulder joint. They help to stabilise your shoulder and provide finely tuned rotational movements to the arm. Injuries to the rotator cuff range from tears and strains to chronic inflammation and overuse injuries.
Rotator cuff injuries can occur at any age. In young adolescents, most injuries to the rotator cuff are caused by overuse (such as during overarm bowling, or painting ceilings) or have a traumatic onset (ie: during a rugby tackle). As we age, incidence increases due to ‘wear and tear’ of the small tendon.
If you have strained or torn your rotator cuff muscles you are likely to get pain and weakness when lifting or rotating your arm. You may also get pain whilst resting or trying to sleep. The range of injuries to this group of muscles is large and they can mimic many other shoulder conditions. It is therefore important to try and get an appointment with your osteopath early in the injury timeline so that they can diagnose the problem and figure out an appropriate treatment plan for you.
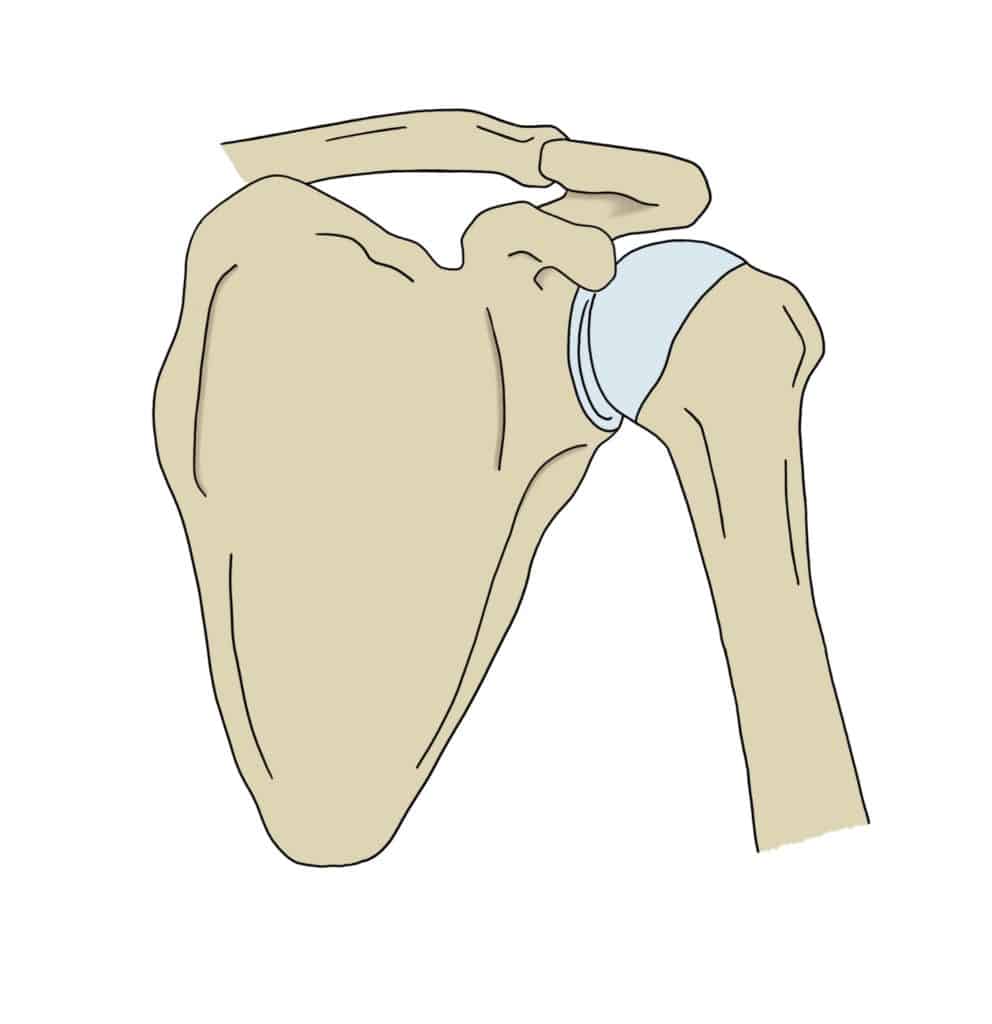
Subacromial Impingement
Subacromial impingement is one of the most common shoulder conditions we see in clinic at The Sussex Osteopaths. It affects one of the tendons of the group of muscles known as the rotator cuff muscles amongst other structures. This tendon passes through a small space at the tip of our shoulder and can become inflamed and painful.
You can also get arthritis and bursitis within the same small space at the tip of the shoulder. Your osteopath will be able to perform specific tests to help diagnose your condition. Subacromial bursitis is often mistaken for frozen shoulder. If you have subacromial bursitis you will experience pain in the shoulder, especially when lifting your arm above your head or lying on the affected side. The pain can radiate down into the arm to the elbow, and worsen with reaching movements or putting on clothing etc.
Our osteopaths are very experienced in treating subacromial impingement and it usually responds well to osteopathy and laser therapy.
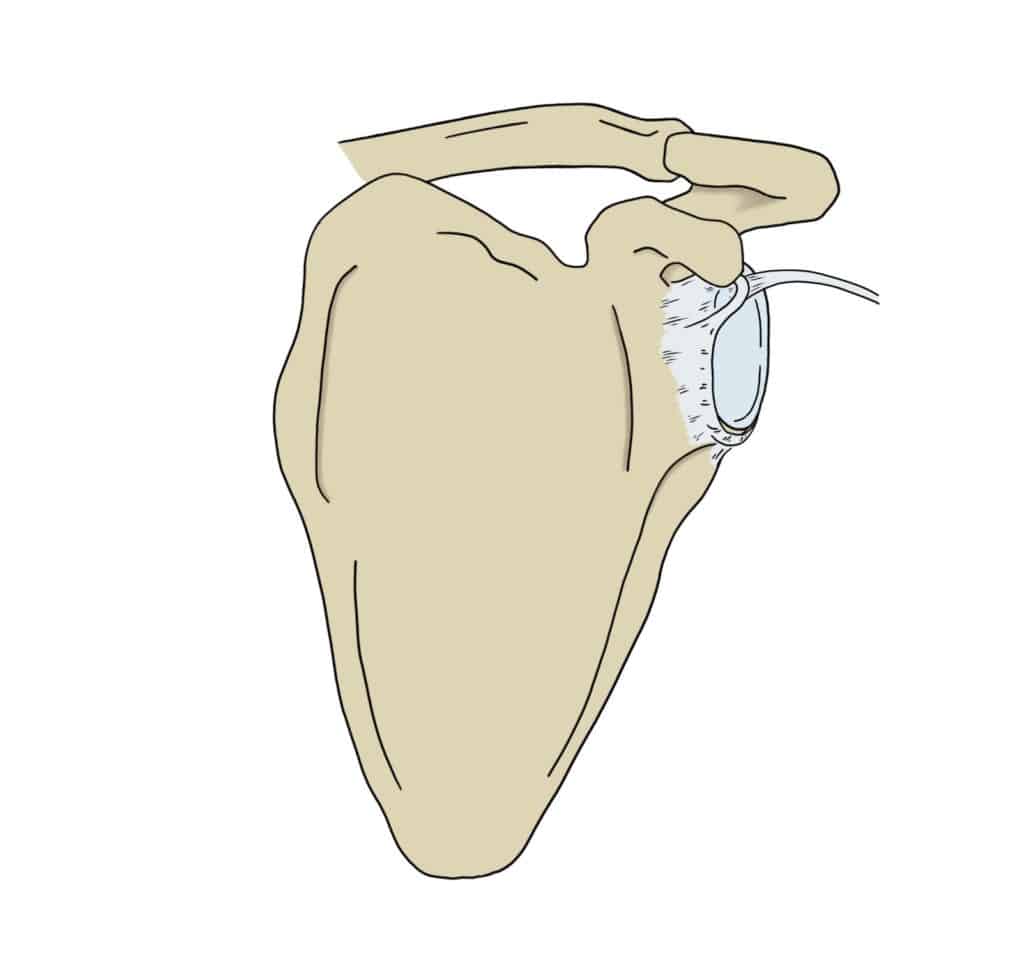
Labral Tear
The labrum is a circular piece of cartilage found in the shoulder joint that helps keep the ball and socket joint in place. A labral tear can occur if the shoulder is involved in a traumatic injury, such as dislocation and repetitive overhead sports such as throwing athletes, but can also occur slowly, fraying over time with age.
You might feel weakness and pain in the shoulder, a clicking or popping sensation and have a reduced range of motion if you tear your labrum. Labral tears can present similarly to many other shoulder conditions.
Your osteopath will perform a series of special tests on the shoulder to come to their diagnosis. In most cases, initial treatment for labral tears involves physical therapy, such as osteopathy to reduce pain, restore function and strengthen the shoulder. If the symptoms do not resolve, your osteopath will be able to refer you for further investigation such as MRI to confirm the diagnosis and see if there is a need for surgery.
Biceps Tendonitis
Biceps tendonitis can occur at either the shoulder or the elbow, but mostly commonly occurs in the shoulder. The long thin tendon sits within a tendon sheath in the upper arm. If it becomes swollen or inflamed it becomes irritated in its confined space within the sheath.
If you have biceps tendonitis you will have pain at the front of your shoulder that may have begun after repetitive movements, but may have come on for no apparent reason. You are more likely to suffer from biceps tendonitis if you play overhead sports, have a previous shoulder injury or have an occupation that requires manual labour.
Biceps tendonitis present similarly to many other shoulder conditions, and often occurs at the same time as a rotator cuff injury. Your osteopath will perform a series of special tests on the shoulder to come to their diagnosis. Initial treatment for biceps tendonitis involves physical therapy, such as osteopathy and laser therapy to reduce pain and inflammation, restore function and strengthen the shoulder.
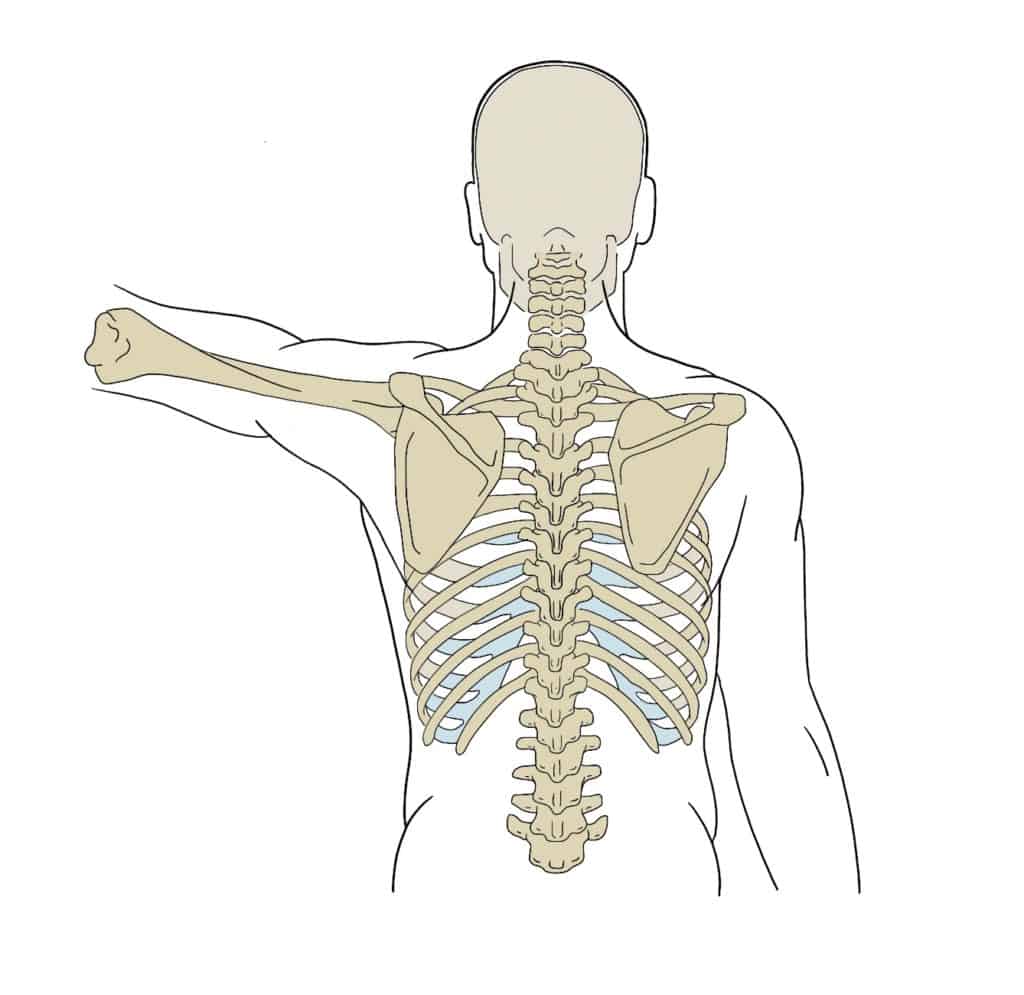
Dislocation
Dislocation of the shoulder joint is almost always as a result of traumatic injury such as a tackle in rugby or fall from a bike. Shoulder dislocations occur more commonly in hypermobile people.
It is one of the most commonly dislocated joints in the body due to its very shallow socket. If you ever dislocate your shoulder, do not try to relocate it yourself. Go to your nearest A&E immediately where they will be able to take an x-ray to check for broken bones and manipulate the arm safely.
You can use a sling or place a pillow between your arm and body to help support the arm until you get medical help.
Once back in the correct position you will need to rest the arm. Laser therapy and osteopathy can then be used to reduce stiffness and pain, reduce inflammation and restore function. We can also help strengthen the shoulder and surrounding structures to help prevent the shoulder dislocating a second time.
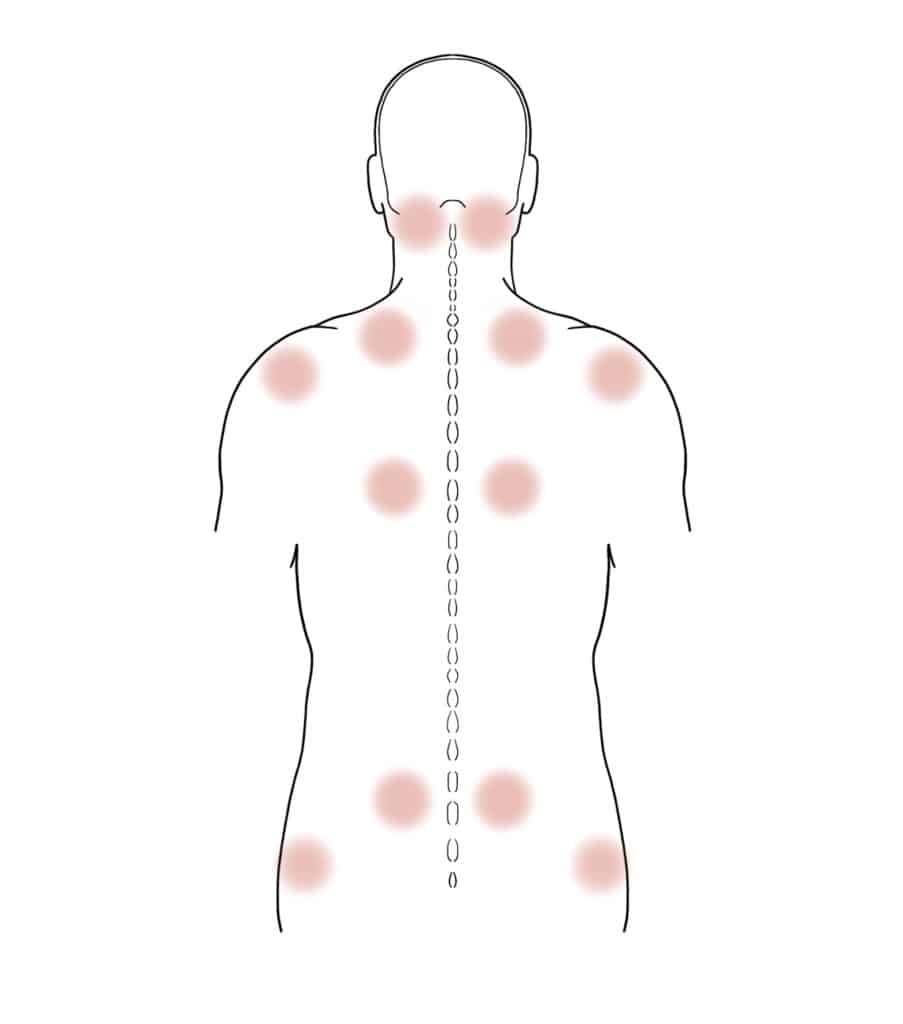
Fibromyalgia
Fibromyalgia is a very complex, long-term condition that causes widespread pain throughout the body.
There is no known cure for fibromyalgia. Exercise is well known to often help relieve symptoms but is sometimes difficult to achieve with the pain levels that patients have to endure. Fibromyalgia is often co-existent with headaches, temporomandibular joint disorders and many other conditions.
Our osteopaths understand and respect the fact that fibromyalgia affects each person differently and adjust their treatment and management approach accordingly. Our aim is to provide much needed relief to the patient in order for them to be able to manage their symptoms and continue every day life activities as much as possible.
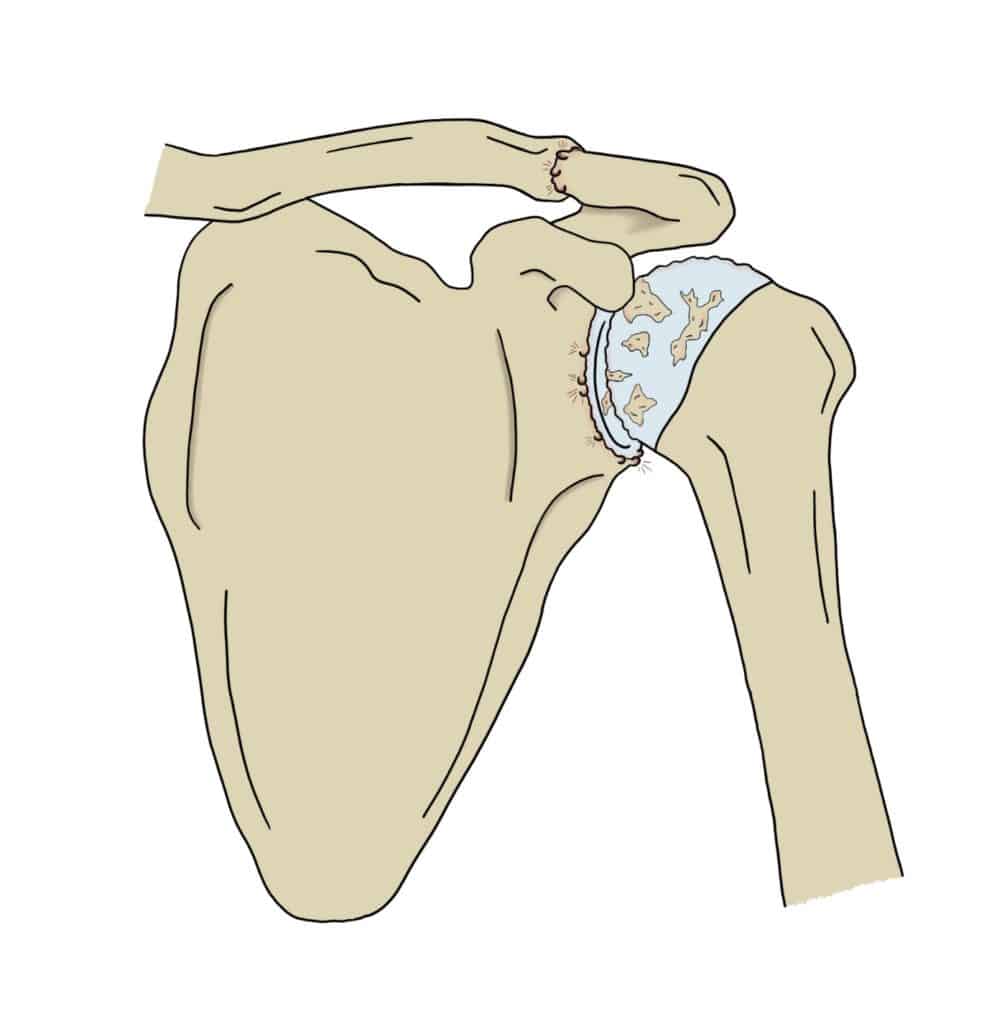
Arthritis
Osteoarthritis is a common condition that causes pain and inflammation in a joint. Often referred to as ‘wear and tear’ of the joint, it can occur at any age as a result of an injury but is most common in people over the age of 45.
The cartilage within the joint becomes thinner, meaning that there is more friction. Osteoarthritis is a normal, natural part of the ageing process and many people with it will suffer no symptoms at all! However, when osteoarthritis is symptomatic, patients complain of stiffness, reduced range of movement and pain on activity.
We can also get a type of arthritis called rheumatoid arthritis; this can affect multiple joints in our body at the same time. If our osteopaths suspect you have rheumatoid arthritis they will refer you to the GP for a blood test to confirm this. We can still treat patients once they have been diagnosed with rheumatoid arthritis and they can get a lot of symptom relief from osteopathic treatment, however it is more complex than osteoarthritis due to it’s nature and usually requires a combined treatment approach with your GP.
There is no cure for osteoarthritis; however, osteopathy can offer symptomatic relief for many patients. Osteopathy can help to increase range of movement available in the joint, decrease pain and improve function. Laser therapy has also been shown to be effective in reducing pain associated with arthritis. We are also able to offer “pre-hab” for those patients awaiting a joint replacement.
Frozen Shoulder
Adhesive capsulitis, or Frozen Shoulder, is a relatively uncommon condition. No one knows why it occurs but having the shoulder still for long periods of time is a risk factor (such as post surgery or long periods using a sling). You are also more likely to get frozen shoulder if you are a woman, over 40 and/or have diabetes.
Many shoulder conditions cause so much pain that the patient is unable to move their arm and they are commonly misdiagnosed as frozen shoulder. Your osteopath will be able to assess you and let you know if they think you have true frozen shoulder.
Unfortunately, true frozen shoulder takes a long time to fully recover and treatment will have a small but limited effect upon it. The timeline of frozen shoulder is split into 3 stages:
- The first 6 months is the ‘freezing’ phase. The shoulder gets gradually more painful and the ability to move it becomes limited. Osteopathy can be used to try and retain as much movement as possible during this stage.
- The second 6 months is the ‘frozen’ stage. The shoulder is very stiff and immobile in this phase, but often a little less painful. We can use the laser to help reduce pain levels but there is not much more that manual therapy can do during this stage other than treat your neck and upper back which may be working hard to compensate for the lack of movement in the shoulder .
- The last stage is the ‘thawing’ phase. The shoulder becomes much les painful and range of movement slowly improves. It can take anywhere from 6-18 months for this final stage to complete. This is where osteopathy can make the most difference. We can help to encourage more movement available, reduce inflammation and restore function and strength to the shoulder and surrounding structures.